Published Feb 26, 2018
Star Trek's Vision of the Future
We're looking at some of the sight restoring technology that Trek has helped to inspire.

StarTrek.com
This series of articles by Edwin Thrower, PhD, will explore how the medical technology seen in the various Star Trek television series and movies may have influenced advances in health and medicine. Many of the devices and therapies described in the episodes have since become reality.
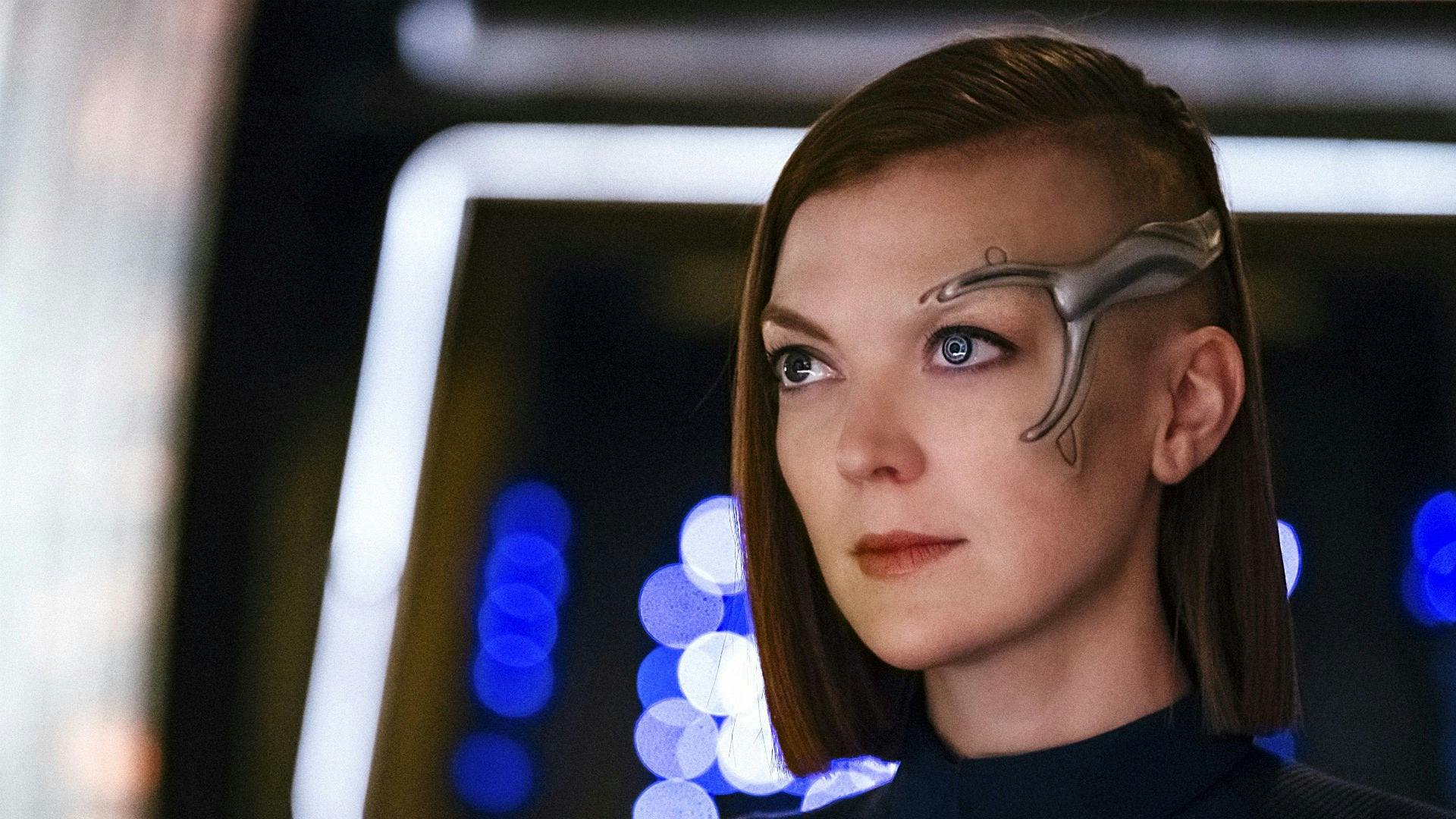
In this first article, we will focus on technologies and medications that’ve been used in Trek to not only improve, but even restore vision. Turning to the latest Star Trek installment, Star Trek: Discovery, Lt. Keyla Detmer serves as helm officer on the U.S.S. Discovery. Detmer has both cranial and ocular implants, a result of being wounded in battle during her time aboard the U.S.S. Shenzhou in the Battle of the Binary Stars. To what extent Detmer can see with her implant is unclear, but we at least know that vision loss can be corrected with 23rd century technology. We’ve also seen other Trek characters use sensory devices to see. In the TOS episode, “Is There In Truth No Beauty?,” Dr. McCoy reveals to a startled Captain Kirk that Dr. Miranda Jones is blind. Dr. Jones has a shawl with a sensor array in it that allows her to “see.” While this device isn’t as effective as Detmer’s implant and does not allow her to see enough to act as an Enterprise pilot, her blindness isn’t perceived by Kirk for much of the episode.
StarTrek.com
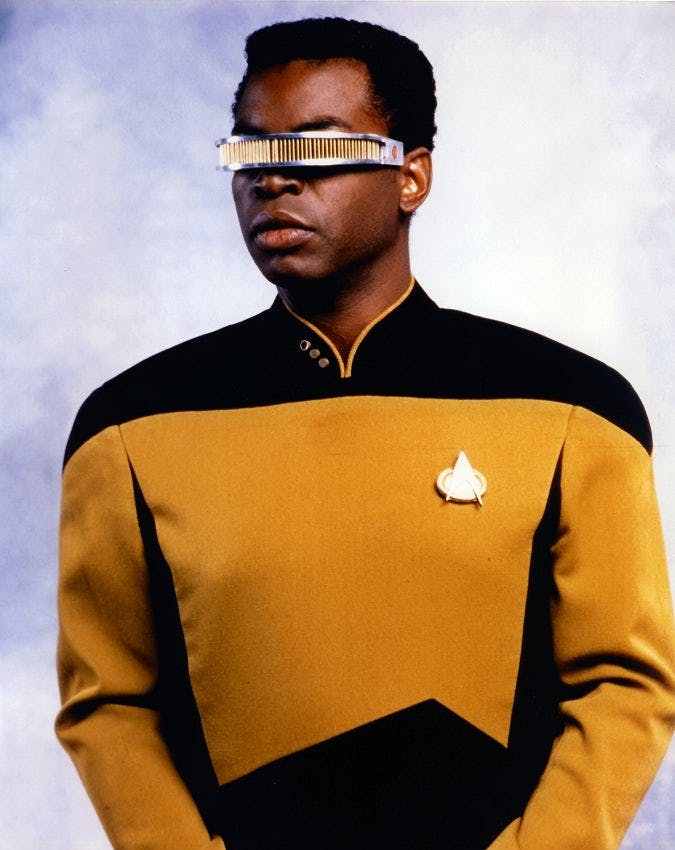
Perhaps the most well-known Trek device for eyesight restoration is the "Visual Instrument and Sensory Organ Replacement," or VISOR, as utilized by Geordi La Forge in Star Trek: The Next Generation. Thanks to the VISOR, blindness is no longer considered a disability by the 24th century. We learn from the TNG episodes "The Naked Now,” "The Masterpiece Society" and "The Enemy" that the VISOR detects electromagnetic signals across the entire EM spectrum between 1 Hz and 100,000 THz and transmits those signals to the brain through neural implants in the temples of an individual via delta-compressed wavelengths. This results in vastly different visual acuity, with VISOR-wearers able to see in the infrared and ultraviolet ranges and beyond.
By 2373, La Forge decided to switch from the VISOR to a pair of ocular implants that resemble the human eye and are distinguished by a vibrant blue color with mechanized detail on the irises and pupils. The implants confer similar benefits to the VISOR in addition to telescopic vision that include heat-detecting infrared capabilities. As with the VISOR, however, side effects include occasional headaches. Also in 2374, the U.S.S. Voyager’s holographic doctor fashioned a custom ocular implant to replace former Borg drone Seven of Nine's cybernetic eyepiece. While the implant was indistinguishable from a normal human eye, the new prosthetic retained Borg components, granting Seven enhanced vision. Seven's implant was even equipped to detect irregularities in space-time!
When TNG first aired, the VISOR may have seemed revolutionary. However, merely 30 years on we’re already seeing the advent of similar technologies. Several VISOR-like devices are in various stages of development to help the visually-challenged. Pixium Vision introduced the IRIS II system in 2016 followed by the next-generation PRIMA system in January 2018. The technology involves sub-retinal implantation of a miniaturized, wireless device linked with special glasses and a small pocket computer to enable the recipient to see. Then there are technologies which don’t require surgery. OxSight, Ltd. have developed Helios smart glasses which have a graphics processing unit installed to enhance images for the partially sighted. In trials, about 30 percent of participants reported a significant, immediate improvement. In addition, there’s the eSight system which displays a full-color, hi-resolution video feed of the surrounding environment on two near-to-eye OLED screens with the user able to fine tune the input to best meet their personal vision needs.
While these devices are clearly revolutionary in the treatment of partial vision and blindness, the emergence of other kinds of medical advancements may leave something as clunky as a VISOR obsolete before we even get to the mid-21st century, let alone the 24th century. Among these new approaches, actual optic nerve or retinal regeneration may prove to be a viable solution.
StarTrek.com
Age-related Macular Degeneration (AMD) is a condition in which the light-sensitive cells of the macula — the central part of the retina — are destroyed. Last year, surgeons inserted a telescope implant manufactured by VisionCare into a patient’s eye. The minute device magnified a small area and projected the image across the whole retina, allowing healthy cells to distinguish the image clearly. This enabled the patient to read again, watch football on television, and even plant a vegetable garden. The VisionCare telescope implant was recently awarded FDA approval for patients 65 and older with end-stage AMD. The device is implanted only in one eye, and the other eye continues to have full peripheral vision. The implant cannot be placed in an eye that has had cataract surgery. As some patients have trouble adjusting to the different images each eye receives, ophthalmologists conduct a series of tests to determine if prospective candidates are a good fit. For most patients, significant improvements have been seen.
Wet macular degeneration occurs when abnormal blood vessels grow under the retina, often leaking fluid or blood into the macula and damaging central vision. A new class of drugs called anti-VEGF agents have emerged and can halt and even reverse the damage. The medications are injected directly into the eye, where they block VEGF proteins, which normally help blood vessels form. In a majority of patients, vision can be stabilized and, in some, restored. The shots have one big drawback: they must be administered monthly. To counter this, researchers are developing innovative ways to deliver medication to the eye. One approach under investigation is implantation of a tiny reservoir that steadily releases medication over time. Another more advanced possibility is the use of gene therapy to reprogram cells in the eye to produce their own anti-VEGF agents.
Perhaps the most-ambitious approach to vision restoration in patients with AMD is eye-cell regeneration. In 2014, a team at the Jules Stein Eye Institute at the University of California, reported early success growing retinal cells in the lab and injecting them into the eyes of patients with different forms of AMD. The scientists began with pluripotent stem cells, which are cells with the capability of becoming any cell. Over several months, the cells are coaxed into becoming retinal pigment epithelial cells, which support photoreceptor cells in the retina. Ocata Therapeutics, a Massachusetts-based company is developing the procedure, and preliminary results demonstrated significant improvements in vision in some patients; clinical trials are now under way to refine the procedure. Using a different methodology, researchers at a California-based company called Eos Neuroscience have successfully inserted a gene that enables cells to capture light. The goal is to engineer healthy eye cells to take over for photoreceptor cells that’ve been destroyed by retinitis pigmentosa or macular degeneration. Experiments in mice have shown promise and clinical trials in humans may follow.
For years, the only treatment for glaucoma, which results from a build-up of pressure within the eye and is a leading cause of blindness among those 60-plus, was medicated eye drops. But getting people to administer drops can prove challenging. Patient surveys indicate that as many as half of people with glaucoma halt their use of eye drops in the first year. As an alternative, Joseph Ciolino, an ophthalmologist at Massachusetts Eye and Ear, part of Harvard Medical School, and his colleague Daniel Kohane, M.D., who directs the Laboratory for Biomaterials and Drug Delivery at Boston Children's Hospital, have developed a contact lens that contains glaucoma medication sandwiched by a thin polymer film. The lens was shown to successfully release a steady and consistent dose of medication for up to a month in studies which were completed last year.
Trek has shown us a future in which visual impairment was a thing of the past. People could lead normal lives due to medical and technological advancements. Thanks to researchers and medics who may have been inspired by Star Trek, our current technology is not only fast approaching that seen onscreen 30-50 years ago, but is actually surpassing it. Star Trek and medicine walk hand in hand; one inspires the other and both result in hope.
Edwin Thrower PhD is a Senior Scientific Specialist at Parexel International and a Senior/Visiting Research Scientist at Yale University.

